#6- THE FINALE
August 15th, 2018 by edwardchristiansen
Posted in Uncategorized|
Profound. Captivating. In-depth. This is what my final post must be. How will it summarize what I’ve learned and best express that to my readers? Usage of action phrasing, colorful verbiage, pattern/intonation… Will it live up to the hype? These questions have been running through my mind since the moment I stepped off the plane in Kansas City Friday after 20+ hours of travel. I was picked up by a colleague who greeted with me with a smile and a hug. “How are you? Are you happy to be home? Tell me what you learned in Africa?”
It is now Monday and I can frankly say these are the first 3 questions every single person has asked me. I shall answer them here so as to best dissuade some others I’ve yet to see from noting my frustration as they’re answered:
1) “How are you?” I’m tired. Jet lag is real and regardless of my abilities throughout residency to change schedules, it has not been easy. I find myself needing a nap just to get through the day. My stomach has not yet adjusted to the diet and my timing is just slightly off when driving my car. I find myself noting more stimuli (e.g. noises, smells, lights, etc.). I tried to hang out with some friends who came into town and I didn’t last past 10pm! In summary, I am a bit rundown.
2) “Are you happy to be home?” Yes! I enjoyed my experience in South Africa but am very glad to be home. I assume this is a lead-in question to what follows but in truth, what person would say no?
3) “Tell me what you learned in Africa?” Are you kidding me? You want me to summarize what I learned? Thus far, I’ve answered this question with one random story, which leads into another story, and so on, and so on, and so on. While entertaining, it actually does not answer the question originally asked. I shall attempt to answer it in the next paragraphs. But what method should be used to in order to start this?
The Blood Moon
My second opportunity to be social found me in a 4×4 with some colleagues heading north towards Nhlamvu and the bush. We would rent some high class tents which had surrounding accommodations for food prep, a fire pit, and toilets/shower. This was all in celebration of the “Blood moon.” This phenomenon is a complete lunar eclipse and occurs when the Earth comes between the sun and the moon. The red color is caused as small amounts of light from the sun are trapped in our atmosphere. As the light bends around the Earth it falls on the moons surface and produces this coloring. The perfect sight for this just happened to be Africa. We arrived and set up camp. This was a pretty posh campground with actual beds, serious reinforced tents, and a full kitchen. There was a bar and a pool. This was awesome. As night fell my inner pyromaniac came out and I took it upon myself to build an awesome fire. I was also tasked with finding a place away from the light of the campground in the bush to view this eclipse. Multiple trips walking through the bush allowed me to find a great spot. It was a small clearing next to two acacia trees (think every African picture you’ve ever seen). The night was still and the stars bright. A light breeze blew in from the sea and the air smelled of fire. Mars was a fire red and lay beside the moon. As the group convened, I was reminded just how small I was in this vast universe. The event was magical and luckily my colleague Remy got some great shots with his nice camera. The following days were filled with amazing experiences. I helped cook and eat ostrich, made friends with others who joined us there, and visited a combination salt water/fresh water lake. Being in the bush was so peaceful and the experience never forgotten.

The beginning of the Blood Moon

Shadow beginning to have it’s effect on the moon

Almost there

The BLOOD MOON. It was eerily beautiful.

Our awesome campsite with serious tents!

Walking back in the evening with the girls to the campsite

The ladies in the morning…

Me being a pyromaniac!

Makeshift raft on the side of this freshwater lake

Lake Pic #2

The Whole Group
The Sardine Run
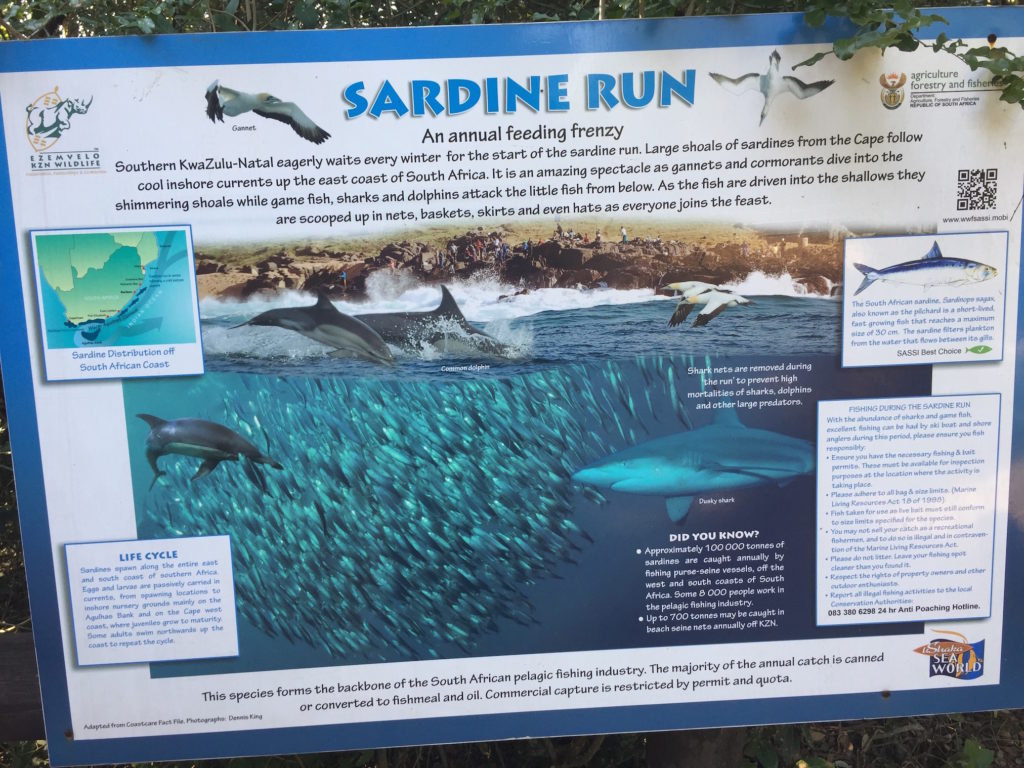
Sign explaining the Sardine Run at Maibibi beach earlier in the trip
If you aren’t familiar with the Sardine Run of South Africa, I recommend watching the BBC’s coverage of it. Surely you’ve seen some of the short clips of dolphins breaking large shoals of fish into “bait balls” as they feed. Sardines, or pilchards, swim in large groups in order to improve survival. It was 0630 and I loaded my bags into Rachel’s car. She had recommended I be taken to the closest large town in order to grab a Taxi to the large city of Durban. There I would check into a hotel for the evening, so I could easily make my flight the following day. On my way into rural South Africa and Mseleni, I grabbed a private taxi at my previous hotel and had received a history lesson, gotten lost, and paid out the nose for it monetarily. Rachel said I could grab a group taxi and get to Durban at a fraction of the previous cost. Not being completely ignorant on what I was in store for, my colleagues I spoke with said it would be a good experience for me. And so, there I was in a town called Mbazwana at a large taxi station. It was early and there was a chill in the air. Large taxis sputtered in and out all around. All of these taxis looked similar; circa 2000, all same model…except mine.

The Taxi and my bags
I sat my bags (one of them incredibly large…in fact, I don’t think Samsonite even sells such a large bag anymore as oil prices have increased since it’s last usage in 1999) in front of the “taxi” and waited for directions. As Rachel and I said our goodbyes, she noted the driver was somewhere else, but to just leave my bags and they would be loaded. I was to hop on the bus, and when the driver saw the bus was full, he would leave. As the bus filled up with more and more people and items, my goliath of a bag remained outside. People climbed in and sometimes over others. 2 hours passed and we were still sitting there; my bag remaining outside. Another hour passed and more people piled in. No way my bag was getting in the van with me. I began to think what’d I do if the door was quickly closed and my bag had not been loaded. I was seated in the very back seat wedged between a very heavyset African hairdresser and the window. The trunk door was behind me and I figured I might be sweaty enough to slither out should it come to it. The driver showed up and looked at my bag. He shook his head and looked in his cab. There was no way it’d fit. Well, necessity is truly the mother of invention. The bag was somehow tetris’d in, money collected, and we speed away at 10am! The final count has 18 people, not including the driver, showed into a small tin taxi with my goliath of a bag and others!

This pic does not do this justice but it was tight to say the least!
At the one hour mark, I noticed I couldn’t feel my butt. Having little to no padding there is a negative when one is sitting on a thin rubber seat with a steel bar somehow supporting it as you barrel down the highway. Every small imperfection in the road abruptly reminding you of its presence at each moment. The kind, yet still obese African hairdresser even more pushed up against me as I feel my left leg begin to go numb. The taxi continues, speeding down the road with no end in sight. The terrain slowly changing from flat small rural estates to large open swathes of sugar cane and hills. A strange combination of body odor, tobacco, and stale must permeates the air. There goes the right leg. This is it…this is my personal Hell. And then I realize it; I simply have to survive. My fellow travelers and I are sardines on a run to Durban. After 4 hours, we pulled up to the central Taxi station in Durban and climbed out of our Sardine tin. I blessed the sea breeze and made my way to my hotel. A shower had never felt so good! An experience to say the least, but one I’d rather not have to have again anytime soon.
Real Life
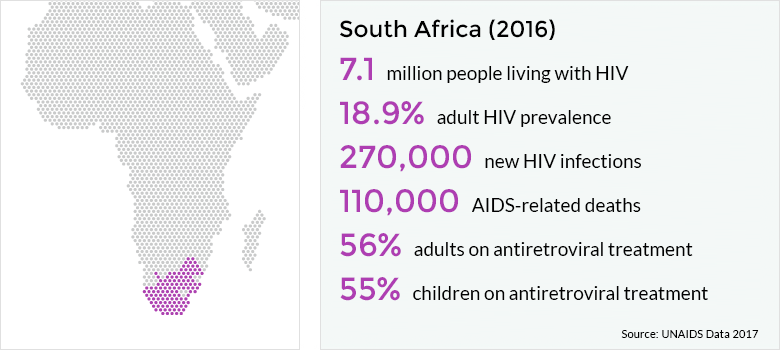
I am pleased to report the total donations collected for this trip will be put towards a very special support group. Called Real Life, this is a part of the Lulisandla Kumntwana program created by Dr. Victor and Rachel Fredlund and is a support group for teenagers living with HIV. In zulu, this means “reach out to the child.” This name is based from James 1:27:
Religion that is pure and undefiled before God the Father is this: to visit orphans and widows in their affliction, and to keep oneself unstained from the world.
As I saw during my time in the area, teenagers represent their own challenges. Psychosocial changes become evident and unfortunately many teens choose to “control” the challenges in their life by withholding their meds. This can create further health issues later including viral resistance. Per Rachel Fredlund, “This group has been meeting for some years and it has been great to see these young people grow, develop, and mature. Some have gone on to tertiary studies and are doing really well. They still keep in touch with and support each other.” She goes on to describe how the group meets once per month and alternating between heavier in-depth discussions and more fun activities. These include boat rides, snorkeling, horse riding, nice meals out, trips to the game reserve, the crocodile farm, and the cat sanctuary. They also have had craft days, cooking days, a newspaper fashion competition, and a dancing day. Twice per year they also have career days for the older teenagers teaching trades and providing information/aid to facilitate educational impact. It is my profound pleasure and honor to give to this crucial group. As its name entails, this support group does just that.
This trip and experience was as much about the people as it was about anything else. Together my faith has been strengthened, compassion and understanding towards other cultures has increased, and my soul has been recharged. While I could not capture all those whom I’ve had the pleasure of meeting, the following will give you an idea of what I had the pleasure of encountering.

Morning coffee and just outside the hospital

Morning at The Fredlund’s. Ahhhh

My morning commute to the hospital

Nightly cooking with Rachel

Singing with the Fredlund’s at Hlulabanthu African Evangelical Church and singing my last phrase “It is well with my soul” in Zulu! An amazing experience
As my search for summation in this, my final blog post, I read numerous articles, books,etc. All seemed to capture aspects of how I feel but never fully encompassed them. The closest I could come is in a sermon by Dr. Albert Schweitzer. Aptly titled First Sermon on Reverence for Life, Dr. Schweitzer captures a necessary duality I once thought I understood.
Desire for knowledge! You may seek to explore everything around you, you may push to the farthest limits of human knowledge, but in the end you will always strike upon something that is unfathomable. It is called life. And this mystery is so inexplicable that it renders the difference between knowledge and ignorance completely relative…
Reverence before the infinity of life means the removal of the strangeness, the restoration of shared experiences and of compassion and sympathy. And thus the final result of knowledge is the same, in principle, as that which the commandment to love requires us. Heart and reason agree together when we desire and dare to be people who attempt to fathom the depths of things.
I have gained a great desire from my passion for helping others. Herein lies another example of how my desire has opened up new opportunities and knowledge into this “unfathomable” thing called life.





































 Hello! My name is Edward Christiansen. I am a Resident Physician at Research Family Medicine Residency, and I’m starting my INMED service-learning experience at Mseleni Hospital in South Africa beginning in July 2018.
Hello! My name is Edward Christiansen. I am a Resident Physician at Research Family Medicine Residency, and I’m starting my INMED service-learning experience at Mseleni Hospital in South Africa beginning in July 2018.