The Public Health Post #5
July 30th, 2018 by edwardchristiansen
Definition
As my journey comes to an end, more needs to be discussed in regards to the public health component of this area. And naturally, as my goal is to obtain an international diploma in Medicine AND Public Health through INMED I shall do so here. The CDC has an excellent definition of public health and it’s many idiosyncrasies. It is defined as the science of protecting and improving the health of people and their communities. This is usually done by promoting healthy lifestyles, researching disease and injury prevention, and detecting, preventing and responding to infectious diseases. In short, public health attempts to protect the health of entire populations.

The Market at the closest town
Data
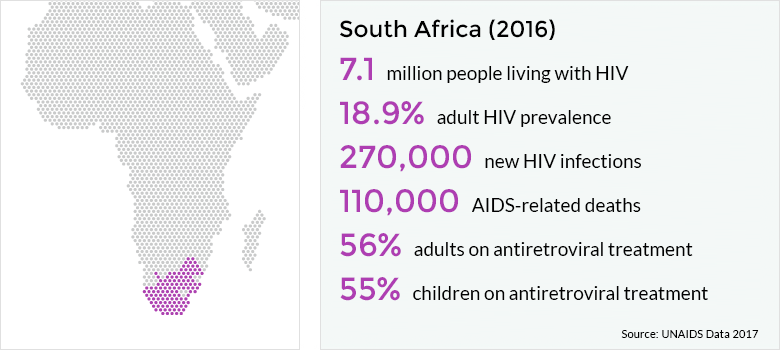
Some data on this community and culture is as follows: The catchment area of this hospital is approximated by Dr. Fredlund who has direct and longstanding knowledge of the area. He estimates the catchment area to be approx. 100,000 people and 40km x15km. The average life expectancy has increased with the advent of ARV’s with its lowest being in the early 1990’s. Now it is estimated at age 50-55. Leading causes of death for men continue to be homicide/battery, HIV, TB, stroke. For women: diarrheal disease, childbirth, abuse/battery, HIV, TB, cervical cancer.


As one can see from the aforementioned numbers, infectious disease continues to be a large portion of the illness affecting this community. Since the advent of ARV’s, life expectancy has increased by approximately 5 years. Much education regarding HIV has bombarded the local youth. HIV remains a rather taboo topic however. Forcible rape, teenage sex/pregnancy can still be found in the societal norms. Law enforcement and the courts are underfunded, underappreciated, and overworked. In summary, education is there but acceptance continues to be an issue.
Mseleni Hospital, which was initially started by Dr. Victor Fredlund and his partner, was handed over to the ministry of health in this province once its size and scope became larger. Mseleni hospital has up to 6 clinics which feed directly to the hospital. Outpatient clinics are essentially run by nurses or “sisters” of varying degrees of education and experience. A pharmacy stockroom, PT room, outpatient surgery, and delivery room are all present. Physicians from the hospital visit each clinic 1-2x per week and are delivered and picked up by a hospital-funded bus. Immunizations are given consistently, but without autonomy. Some patients are transported to the clinics. Any testing ordered by the physician requires the patient to travel to Mseleni Hospital (including obtaining an xray).
Mseleni Hospital contains the following wards with a constantly changing amount of beds/patient’s served: Male ward, male TB ward, maternity, well antenatal, ill antenatal, ill neonatal/highcare, well neonate, postpartum, Female ward, post-op step down, Female TB ward, adult high care, pediatric, Outpatient department/Urgent Care.
Funding, Staffing, and Community Acceptability
Funding is always a major issue. During my short stay here, the largest issue seems to be nursing and the funding therein. As many things in Africa, there is a large problem with lack of consistency of payscales. I’ve experienced nurses here having little to no interest in maximizing their efficiency, clinical skills, etc. Depending on the nurse, many wards do not receive medicines as ordered or at all. Ancillary staff seem to be better situated. The OR is surprisingly clean, however hand sanitizer is always at a premium. In regards to community acceptability, patient’s seem to be respectful, and appreciate the care received at this facility. There still exists a component of “old-time” medicine. Many of our patients come in in unexplained renal failure likely secondary to usage of “traditional medicines.” I’ve asked around and the consensus on what this consists of is anything and everything. One example is a cellulitic wound where “scratching” or taking a razor blade to the skin and cutting superficial lines to “relieve the pressure.” Any solvent available which is caustic (think battery acid or bleach) is then rubbed into the skin. Education is a key component at Mseleni as they continue to aid in attending to this community in need.
Only recently have I encountered some of the difficulties with medicine acceptance in this South African community. Please note, I intend to generalize in the following statements. My information was obtained from Zulu inhabitants/peoples who were kind enough to enlighten me on some of there closely held beliefs and customs. Naturally, not all Zulu people here or in other places believe this way. My statements and discussion therein are meant only to further elucidate areas of study to improve public health and do not represent judgments on my, or other’s behalf. With this being said, Zulu culture seems to be grounded in a fear-based system where luck plays a major component. This luck, bad or good, has a great deal to do with ones ancestors. If your prayers to your ancestors do not avail one of whatever affliction is occurring, you are to visit a traditional medicine doctor/shaman. He is able to speak to them and offer a solution to which ever relative is upset with you. Many times this includes sacrificing of animals(usually a goat) and doing something with certain body parts. If this does not work after a period of time, you are meant to return to the traditional medicine doctor and repeat as necessary.

Example akin to what is seen around the area
Questions to be Answered
How does one not demean cultural/religious beliefs while encouraging allopathic medicine and more scientific practices in things such as sanitation, sex/relationships, etc.? Education still needs to be the key to this puzzle. However, where many come with good intent, personal biases, cultural norms, and ignorance muddy the waters of lasting change. Partnership needs to exist between trusted community leaders and a group. Only then can education be effectively implemented.
Why are poverty and illness/ill-health related? Like anything in this world, medicine and medical care is a service and in order to continue employment of millions, encourage the best and brightest/compassionate of us to enter it, an exchange of compensation must be incorporated. 3rd world countries, as well as 1st, continue to struggle with this model or any model therein. Is medicine a right or is it a business?
Poverty has ever-reaching socioeconomic impact not just in medical care. However, ways in which this was particularly evident during this time was in one main example; transportation. Transportation between towns, hospitals, or even homes is poor. There are not enough busses, ambulances, or even taxis to bring care to those in need. Services are directly influenced by this in KwaZulu-Natal region. Ill infants suffering from sepsis wait while a 34yo with a non-emergent URI is picked up in a surrounding village on the way to the OPD. Elderly end stage renal disease, multiple comorbidity patients are discharged from large hospitals in urban areas (with many more resources) back to their villages. This is done by these facilities even with the knowledge she will ask to be taken directly to a rural hospital to receive a higher level of care than can be obtained at home. This creates a drag on an already fragile, underfunded health system further allowing those who require emergent care to wait on chronic/non-emergent patients prior to obtaining medical care.

OPD-Outpatient Department
Summary and Further Musings
Answers to these questions are complex and require continued study and support. This is in the form of large agencies with good distribution networks and staffing, funding from countries/governments/individuals, and caring/compassionate humans of this planet. Frustratingly, the above questions have been asked for far too long and more recent political/cultural trends place world health in the crosshairs of destruction. One of the greatest threats to world health today is Isolationism. Currently, we are seeing a rise in nationalism/isolationism among many of the world countries. As the U.S. makes up a large portion of the WHO budget and other healthcare budgets, this movement threatens to drastically decrease or cut off funding for many of the worlds underdeveloped regions. With a consistently increasing globalized world, isolationism is no longer a solution to any form of protectionism. If anything, it represents a real and present danger to the health of our own citizens and, just as importantly, the citizens of the world.

I am greatly pleased with the public, authentic isolation in which we two, you and I, now find ourselves. It is wholly in accord with our attitude and our principles.
-Karl Marx


Sorry, comments for this entry are closed at this time.