This 63-year young woman arrived at CEML Hospital 3 days ago with large, full-thickness pressure ulcers of her entire buttock and hips. She was febrile, unconscious, and with a leukocytosis. Her lower extremities were both flaccid and without reflexes. We immediately initiated sepsis treatment with IV fluid and antibiotic therapy.
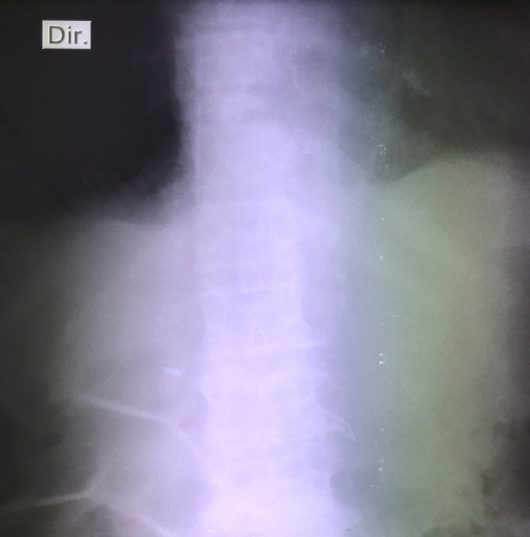
The patient’s family explained that a year ago this woman suffered a “stroke” that left her with “paraplegia” and paralysis of her legs. Attached is the X-ray of her spine. What is your diagnosis?
First of all, with very rare exception, stroke/cerebral vascular accident causes hemiplegia (paralysis of one side of the body) – not paraplegia (paralysis from one level downward). Paraplegia is usually due to disease of the spinal cord, and hence the special usefulness of this X-ray. What do you see? The T-11 vertebra, second from the top, is quite short compared with T-10 above and T-12 below. This T-11 finding correlates with the level of our patient’s paraplegia.
While we treat her sepsis and pressure ulcers, we are also considering the cause of her T-11 collapse. Enter another clue: Our patient’s ESR (erythrocyte sedimentation rate) is 90, about ten times normal. TB is extremely common in Angola, and the organism has special propensity to grow in the spine. While we have no bacteriology to prove this diagnosis, the finding of a high ESR is consistent with TB. So our empirical diagnosis is spinal TB, and our patient is now receiving the four drug TB treatment protocol. Over the coming weeks, a recession of her ESR – and possibly improvement of her paralysis – would be indirect evidence that the diagnosis is correct.