“You plan to work in Africa?” questioned the health education professional at my interview. His tone was decidedly skeptical. “Then why first do medical residency training? Why don’t you just go now?” This attitude is not isolated. Throughout our health professions is the pervasive image that healthcare for people of lesser means should not require the same standard of training or care expected for those who are more wealthy or more familiar to us.
On the balance, health resources available to those who are minorities, low-income, chronically ill, and victims of war or disaster are often less, much less. But should we agree that it’s acceptable for healthcare professionals advocating for such people to themselves be less prepared or qualified? I believe not.
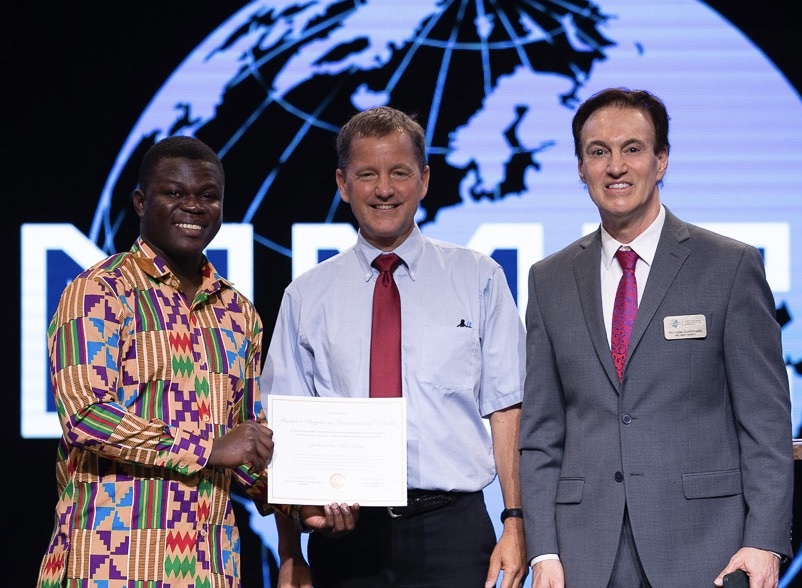
Formal healthcare education and credentials are important. They validate skill to potential partners and employers. They confirm expertise to governments and authorities. Psychologically, they affirm the commitment and the mission of the professional. Socially, credentials help to foster communities among those who share similar experiences, communities that often prove profoundly encouraging.
We at INMED are committed to filling the gaps in traditional education so that healthcare professionals are prepared for unique needs of people who are forgotten, undereducated, disabled, elderly, veterans, refugees, and migrants. Each INMED Credential – including next month’s Hands-On Skills Professional Qualification Courses – earns graduate credit and/or continuing medical education hours.
A few years later I was applying for a medical license in the nation of Ghana – a nation where malaria is the leading cause of death. The government agent asked to see my medical residency training credential. “Oh, excellent,” he replied, examining the document. “We wouldn’t permit anyone less qualified to serve our citizens of Ghana.”