 Andre was just five years young when his parents brought him to a clinic in Africa. As I examined Andre, his parents described weeks of diarrhea and fever. Without appetite, Andre was also rapidly losing weight. On examination of Andre’s chest, I found pneumonia and on his skin, unusual growths. We treated Andre for his infection and dehydration, but after just a few days, Andre succumbed to the mysterious illness. Weeks later, I learned the result of Andre’s blood tests. The baffling disease that plagued his body was actually HIV and AIDS. Without the resources to test or treat this disease, we had little chance of saving this child’s life.
Andre was just five years young when his parents brought him to a clinic in Africa. As I examined Andre, his parents described weeks of diarrhea and fever. Without appetite, Andre was also rapidly losing weight. On examination of Andre’s chest, I found pneumonia and on his skin, unusual growths. We treated Andre for his infection and dehydration, but after just a few days, Andre succumbed to the mysterious illness. Weeks later, I learned the result of Andre’s blood tests. The baffling disease that plagued his body was actually HIV and AIDS. Without the resources to test or treat this disease, we had little chance of saving this child’s life.
Stories similar to Andre’s are myriad. Global attention is riveted on the HIV/AIDS crisis, and rightly so. While progress against HIV is front-page news in wealthier nations, the seldom-mentioned truth is that 95 percent of the people infected with HIV live in developing nations, like Ghana, Africa (UNAIDS/WHO AIDS Epidemic Update: December 2006).
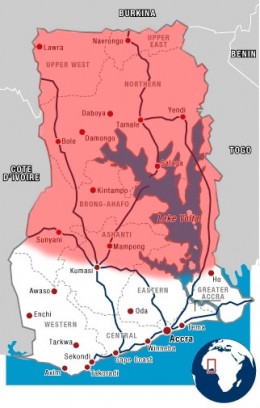
Ghana is an English-speaking nation of 10 million people in West Africa, about the size and shape of Alabama. To the south is the Atlantic Ocean, and to the north the Sahara Desert. Soon after discovery by Europeans, Ghana was used as a rich source of slaves. Today, Ghana is a democracy struggling against poverty and ill health. In Ghana as a whole, the prevalence of HIV infection is about 4 percent (UNAIDS/WHO Epidemiological fact sheet – 2002 Update). Ghana’s Ministry of Health projects, however, that prevalence rate could increase to 9.0% by 2014, giving a total number of infected Ghanaians to be about 1.2 million (National AIDS/STI Control Programme, 2001). The southern portion of Ghana is home to the capital city, Accra, and to an HIV intervention. However, northern Ghana is geographically remote and more impoverished. Like many parts of the developing world, today there is no HIV intervention in the northern two-thirds of Ghana – home to about 3 million people.
The dire growth of HIV in developing nations like Ghana tempts some people to deem the problem hopeless. This perspective, however, is not justified. Consider these facts:
• Simple HIV testing reduces risk of HIV. A research study in Kenya, Tanzania and Trinidad found that people offered HIV testing were significantly less likely to engage in high-risk sexual behavior (UNAIDS, “The impact of Voluntary Counseling and Testing, 2001).
• HIV treatment protects newborns. 35-45 percent of HIV-infected pregnant women will transmit the infection to their newborn babies. But with testing and simple drug therapy this risk can be reduced to just 2-3 percent (Resource-Poor Guidelines: WHO, 2004).
• HIV drug therapy is effective. Provision of HIV drug therapy can be accomplished at low cost while prolonging life and reducing disease complications (Cost-Effectiveness of HIV Treatment in Resource-Poor Settings: NEJM, 2006)
Often what most hampers successful interventions like these is lack of leadership. Effective strategies and funding can be brought to bear against HIV – but only by those who are motivated and equipped to do so. INMED is moving forward to fill this need for trained HIV leaders. Through these efforts, we can touch lives with compassion. We can protect the next generation. We can save another child from HIV.
