 “Doctor, I feel awful: burning up, terrible chills, aching throughout my body, vomiting, massive fatigue. I can’t care for my children. Going to work is unthinkable. How did this happen?” When I am not at INMED, I practice emergency medicine. On a 12-hour shift this week I saw 18 patients, and seven – like this woman – tested positive for influenza.
“Doctor, I feel awful: burning up, terrible chills, aching throughout my body, vomiting, massive fatigue. I can’t care for my children. Going to work is unthinkable. How did this happen?” When I am not at INMED, I practice emergency medicine. On a 12-hour shift this week I saw 18 patients, and seven – like this woman – tested positive for influenza.
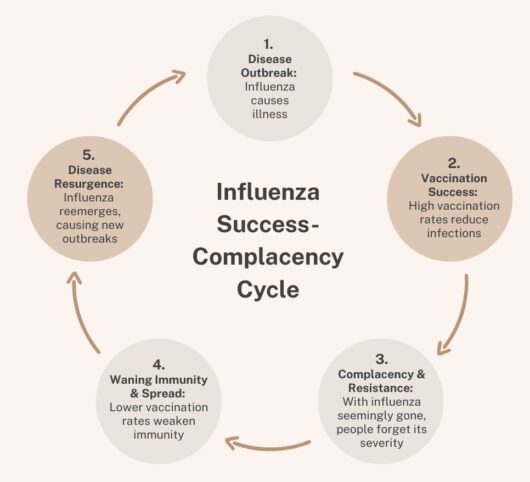
What is the Influenza Success-Complacency Cycle?
1. Disease Outbreak: Influenza causes illness. 15-22 million civilians and soldiers perished in World War One. At roughly the same time, 1918, 50-100 million people worldwide died from influenza. Why is this relevant? Because most people now days have forgotten what a deadly disease is influenza. Even today, 300,000-600,000 die each year from influenza mainly among children under five in nations of Africa and southern Asia who don’t routinely vaccinate them.
2. Vaccination Success: High vaccination rates reduce infections. Development of influenza vaccine is the most important advance in control of this disease. Vaccination reduces hospitalization by about 70% and death by about 85%. But the influenza virus predictably changes overtime, and influenza vaccine must be updated regularly to maintain effectiveness. High public vaccination rates, plus antiviral treatment for influenza illness, is largely responsible for control of this disease
3. Complacence & Resistance: With influenza seemingly gone, people forget its severity. Misunderstandings about how vaccines work, concerns about side effects, the need for an annual updated vaccine, and misinformation contribute to declining vaccination against influenza. One of the most common misunderstandings is that many people’s natural immunity is not sufficient to survive the disease. Healthy lifestyle alone did not protect those 50-100 million people who died in 1918. Not until the supplemental immunity that results from vaccination did influenza come under control.
4. Waning Immunity & Spread: Lower vaccination rates weaken immunity. As vaccination coverage declines, community-level protection weakens, allowing the virus to spread more easily to those at highest risk — including infants, older adults, and people with compromised immune systems. While individuals and parents must retain ultimate authority about being vaccinated, the virtuous choice is to be vaccinated to not transmit the disease to these most vulnerable people.
5. Disease Resurgence: Influenza reemerges, causing new outbreaks. Many communities throughout North America and around the globe are experiencing a surge in influenza, leading to more hospitalizations and greater strain on healthcare services. Schools, workplaces, and long-term care facilities are especially affected, since influenza spreads quickly in close-contact settings. This resurgence is our reminder that influenza remains a serious disease, not just a seasonal inconvenience.
“What should I do now?” asked my ER patient? Together, we discussed rest, fluids, analgesics, anti-viral medication, and avoiding contact with others. “And when I can get the influenza shot?” she inquired. “Just as soon as your fever and symptoms are gone, stop by your pharmacy. Flu season may last until May, so it’s not too late.”
